Introduction
The History of Pharmacy in India has evolved over thousands of years. From ancient practices like Ayurveda to modern pharmacopoeias and drug regulations, the journey has been vast and significant.
This blog explores the complete History of Pharmacy in India, including traditional systems, legal milestones, and the role of pharmacopoeias in shaping the industry.
Topics Covered
- Traditional medical systems
- Emergence of modern pharmacy education
- Legal reforms
- Development of pharmacopoeias (IP, BP, USP)
- Growth of pharmacy as a profession
Ancient Roots of Pharmacy in India
Ayurveda
The History of Pharmacy in India begins with Ayurveda, which originated during the Vedic period around 5000 years ago. Main texts like Charaka Samhita and Sushruta Samhita guided Vaidyas in preparing medicines using herbs, minerals, and animal products.
Siddha
Siddha medicine originated in Tamil Nadu. It was practiced by Siddhars who believed in natural healing and spiritual balance.
Unani
Unani was introduced in India by Arabs during the Mughal era. Hakims practiced it based on the theory of four humors and used plant and mineral-based remedies.
Homeopathy
Homeopathy entered India in the early 19th century through European missionaries. It gained popularity for being affordable and is now regulated under the Ministry of AYUSH.
These traditional systems form the foundation of the History of Pharmacy in India, showcasing the depth of indigenous knowledge.
The Pre-Regulatory Era: No Laws, No Standards
Before independence, the History of Pharmacy in India lacked formal laws and quality standards. Medicines varied in composition, and there was no regulatory body to ensure drug safety.
Most practitioners either followed traditional texts or foreign standards like the British Pharmacopoeia. This unregulated environment made drug safety a major concern.
Role of Pharmacopoeias in Indian Pharmacy
A pharmacopoeia is an official standard-setting document for drugs. It ensures identity, purity, strength, and safety of medicines.
British Pharmacopoeia (BP)
Introduced in 1864, it was widely used during colonial rule and influenced early practices in the History of Pharmacy in India.
United States Pharmacopeia (USP)
Though not official in India, USP is referenced by Indian pharmaceutical companies to meet global standards.
Indian Pharmacopoeia (IP)
The first Indian Pharmacopoeia was published in 1955. It played a major role in modernizing the History of Pharmacy in India by offering national standards for drug formulation.
The IP was a game-changer in the History of Pharmacy in India, offering India-centric drug standards.
Indian Pharmacopoeia (IP)
| Year | Edition/Update | Key Highlights |
|---|---|---|
| 1946 | Indian Pharmacopoeial List | Foundation list for official Indian Pharmacopoeia. |
| 1955 | First Edition | Official publication, standards for drugs established. |
| 1960 | Supplement of IP 1955 | Updates and corrections to the first edition. |
| 1966 | Second Edition | Updated standards and revisions. |
| 1975 | Supplement of IP 1966 | Updates and corrections. |
| 1985 | Third Edition | Published in two volumes: Volume I (A–P) and Volume II (Q–Z). |
| 1989 | Addendum I to IP 1985 | New revisions and updates. |
| 1991 | Addendum II to IP 1985 | Further revisions. |
| 1996 | Fourth Edition | Updated standards and new monographs. |
| 2022 | Ninth Edition | Latest drugs and pharmaceutical standards included. |
| 2024 | IP Addendum 2024 | New monographs added to IP 2022 (Source) |
British Pharmacopoeia (BP)
| Year | Edition/Update | Key Highlights |
|---|---|---|
| 1864 | First Edition | Official publication, drug standards established. |
| 1926 | Establishment of BP Commission | Formation of commission to prepare new editions. |
| 1932 | New Edition | Updated standards and revisions. |
| 1968 | Medicines Act 1968 | BP Commission reconstituted for new editions. |
| 1980 | 13th Edition | Updated standards. |
| 1988 | 14th Edition | Updated standards. |
| 1993 | 15th Edition | Updated standards. |
| 2023 | Latest Edition | Includes 23 new BP monographs, 59 new Ph. Eur. monographs, 151 revised BP monographs (Source) |
United States Pharmacopoeia (USP)
| Year | Edition/Update | Key Highlights |
|---|---|---|
| 1820 | First Edition | Official publication, drug standards established. |
| 1888 | National Formulary (NF) Established | Foundation for standardized drug quality alongside USP. |
| 1974 | NF Acquired by USP | Integration of NF into USP standards. |
| 1980 | USP-NF Combined Edition | Combined publication of USP and NF standards. |
| 2023 | USP 46 – NF 41 | Latest edition covering drugs, biologics, dosage forms, excipients, medical devices, dietary supplements, and other pharmaceutical standards (Source) |
Each edition reflects a milestone in the History of Pharmacy in India, improving drug regulation and safety
Beginning of Modern Pharmacy Education
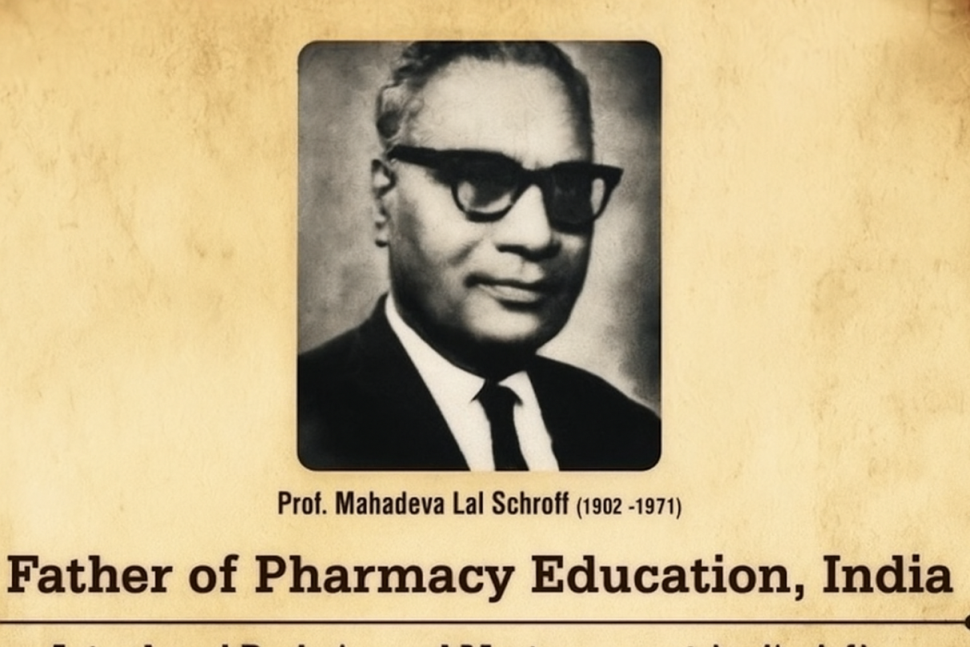
The academic side of the History of Pharmacy in India began with Prof. M. L. Schroff, known as the Father of Indian Pharmacy Education.
- Initiated the first B.Pharm course in 1937 at Banaras Hindu University
- Shifted pharmacy from a traditional to a scientific profession
Legal Reforms in Indian Pharmacy
The legal framework reshaped the History of Pharmacy in India, bringing order and accountability to the field.
Drugs and Cosmetics Act, 1940
- Regulated manufacture, labeling, and distribution
Pharmacy Act, 1948
- Established the Pharmacy Council of India
- Made pharmacist qualification and registration mandatory
Growth and Revolution in Pharmacy Education
| Period | Development |
|---|---|
| Pre-1940 | No formal education |
| 1937 | First B.Pharm at BHU |
| 1948–1970s | Legal structure established |
| 1980s–1990s | Pharmacy colleges expanded |
| 2000s–Today | Pharm.D, clinical pharmacy, R&D |
This academic evolution is a vital chapter in the History of Pharmacy in India.
Modern Indian Pharmacy: Scope and Structure
| Parameter | Then | Now |
|---|---|---|
| Education | Informal | PCI-recognized programs |
| Legal Standards | Absent | Drugs & Cosmetics + Pharmacy Act |
| Drug Quality | Unregulated | Guided by IP, GMP, CDSCO |
| Practice Systems | Ayurveda, Unani | Integrated with modern systems |
| Institutions | None | PCI, IPC, CDSCO, NIPER, AYUSH |
History of Pharmacy in India
In ancient India the sources of drugs were of vegetable, animal and mineral origin. They
were prepared empirically by few experienced persons. Knowledge of that medical system was
usually kept secret within a family.
There were no scientific methods of standardization of drugs.
Muslim rule in India
The Indian system of medicine declined during the Muslim rule while the Arabic or the Unani-Tibbi system flourished.
British rule in India
The western or the so-called Allopathic system came into India with the British traders who later
become the rulers. Under British rule this system got state patronage. At that time it was meant for
the ruling race only. Later it descended to the people and become popular by the close of 19th
Century.
Before 1940
Initially, all drugs were imported from Europe. Gradually, the manufacturing of some of these drugs began in India.
- 1901: Establishment of the Bengal Chemical and Pharmaceutical Works in Calcutta by Acharya P.C. Ray.
- 1903: A small pharmaceutical factory was set up at Parel (Bombay) by Prof. T.K. Gujjar.
- 1907: Alembic Chemical Works was established in Baroda, again by Prof. T.K. Gujjar.
During this time, drugs were mostly exported in crude form and imported in finished form.
The situation worsened during World War I (1914–1920), when drug imports were completely cut off. After the war, imports resumed, but in the absence of any quality control laws, foreign manufacturers took undue advantage.
The consequences were serious:
The markets were flooded with useless and harmful drugs, often sold by unqualified individuals.
Inferior and adulterated medicines were dumped in the Indian market by foreign manufacturers.
Examples of maladies:
- Poisoning due to quinine.
- Putting of croton oil into eye instead of atropine solution.
- Selling of chalk powder tablets in place of quinine.
- Drug santonin was badly adulterated.
- Potent drugs like compounds of antimony and arsenic and preparations of digitalis were dispensed without any standard.
Few laws were there having indirect bearing on drugs, but were insufficient:
- 1878 Opium Act – Dealt with cultivation of poppy and the manufacture, transport, export, import and sale of opium.
- 1889 Indian Merchandise Act – Misbranding of goods in general
- 1894 Indian Tariff Act – Levy of customs duty on goods including foods, drinks, drugs, chemicals and medicines imported into India or exported therefrom.
- 1898 Sea Customs Act – Goods with ‘false trade description’ were prevented from importing under this act.
- 1919 Poisons Act – Regulated the import, possession and sale of poisons.
- Indian Penal Code – Some sections of IPC have mention of intentional adulterations as punishable offence.
Some State-Level Laws with Indirect References to Drugs
- 1884 – Bengal Municipal Act
- 1901 – City of Bombay District Municipal Act (Concerned with food)
- 1909 – Bengal Excise Act
- 1911 – Punjab Municipal Act
- 1912 – United Provinces (now Uttar Pradesh) Prevention of Adulteration Act
Refers to adulteration of foods and drugs - 1914 – Punjab Excise Act
- 1916 – United Provinces Municipalities Act
Inspection of shops and seizure of adulterated substances - 1919 – Bengal Food Adulteration Act
- 1919 – Bihar and Orissa Prevention of Adulteration Act
- 1919 – Madras Prevention of Adulteration Act
Chiefly concerned with food adulteration - 1922 – Bihar and Orissa Municipal Act
- 1922 – Central Provinces Municipalities Act
- 1925 – Bombay Prevention of Adulteration Act
- 1929 – Punjab Pure Food Act
The laws were too superficial and had indirect link to drugs.
Drug Enquiry Committee
On 11th August 1930, the Government of India appointed a committee under the chairmanship of Late Col. R.N. Chopra to examine the problems of pharmacy in India and recommend necessary measures. The committee submitted its report in 1931.
The report revealed that there was no recognized or specialized profession of pharmacy in India. Instead, a group of people known as compounders were informally handling pharmaceutical responsibilities.
Following the report, Prof. M.L. Schroff (Mahadeva Lal Schroff) initiated pharmaceutical education at the university level in Banaras Hindu University (BHU).
In 1935, the United Province Pharmaceutical Association was formed, which later evolved into the Indian Pharmaceutical Association (IPA).
The Indian Journal of Pharmacy was started by Prof. M.L. Schroff in 1939. The All India Pharmaceutical Congress Association was established in 1940, and the Pharmaceutical Conference began holding sessions at various locations to promote the pharmacy profession.
- 1937: Government of India introduced the Import of Drugs Bill, which was later withdrawn.
- 1940: The Drugs Bill was introduced to regulate the import, manufacture, sale, and distribution of drugs in British India. It was later adopted as the Drugs Act of 1940.
- 1941: The Drugs Technical Advisory Board (D.T.A.B.) was constituted. The Central Drugs Laboratory was also established in Calcutta.
- 1945: The Drugs Rule under the Drugs Act of 1940 was framed. This Act has been amended several times and currently includes provisions for Cosmetics, Ayurvedic, Unani, and Homeopathic medicines.
- 1945: The government introduced the Pharmacy Bill to standardize pharmacy education in India.
- 1946: The Indian Pharmacopoeial List was published under the chairmanship of Late Col. R.N. Chopra. It included drugs used in India that were not listed in the British Pharmacopoeia.
- 1948: The Pharmacy Act was passed.
- 1948: The Indian Pharmacopoeial Committee was constituted under the chairmanship of Dr. B.N. Ghosh.
- 1949: The Pharmacy Council of India (PCI) was established under the Pharmacy Act.
- 1954: Education Regulations were implemented in some states, while others lagged behind.
- 1954: The Drugs and Magic Remedies (Objectionable Advertisements) Act was passed to prevent misleading medical advertisements (e.g., cure-all pills).
- 1955: The Medicinal and Toilet Preparations (Excise Duties) Act was introduced to enforce uniform excise duties for alcohol-based products.
- 1955: The first edition of the Indian Pharmacopoeia was published.
- 1985: The Narcotic and Psychotropic Substances Act was enacted to control the abuse of addictive drugs.
The Government of India continues to regulate drug pricing in India through the Drugs Price Control Orders (DPCO), which are updated periodically.
Code of Ethics as Drafted by Pharmacy Council of India (P.C.I.)
Ethics is defined as ‘code of moral principles’. It emphasizes on the determination of right
or wrong while doing one’s duty.
Code of Pharmaceutical Ethics as formulated by Pharmacy Council of India which are
meant to guide the pharmacist as to how he should conduct himself (or herself), in relation to
himself (or herself), his / her patrons (owner of the pharmacy), general public, co-professionals etc.
and patients.
Introduction:
Profession of Pharmacy is a noble profession as it is indirectly healing the persons to get
well with the help of medical practitioners and other co-professionals. Government has restricted
the practice of Pharmacy to only Profession Pharmacists i.e registered Pharmacist under the
Pharmacy Act 1948. PCI framed the following ethics for Indian Pharmacists, which may be
categorised under the following headings:
- Pharmacist in relation to his job.
- Pharmacist in relation to his trade.
- Pharmacist in relation to medical profession.
- Pharmacist in relation to his profession.
Pharmacist in relation to his job
A pharmacist should keep the following things in relation to his job.
(i)Pharmaceutical services
Pharmacy premises (medicine shops) should b e registered. Emergency medicines and common
medicines should be supplied to the patients without any delay.
(ii)Conduct of the Pharmacy
Error of accidental contamination in the preparation, dispensing and supply of medicines
should be checked in a pharmacy.
(iii)Handling of Prescription
A pharmacist should receive a prescription without any comment on it that may cause anxiety
to the patient. No part of the prescription should be changed without the consent of the
prescriber. In case of changing the prescription should be referred back to the prescriber.
(iv)Handling of drugs
A prescription should always be dispensed correctly and carefully with standard quality drug
or excipients. Drugs that have abusive potential should not be supplied to any one.
(v)Apprentice Pharmacist
Experienced pharmacists should provide all the facilities for practical training of the apprentice
pharmacists. Until and unless the apprentice proves himself or herself certificate should not be
granted to him / her.
Pharmacist in relation to his trade
Following are the provisions which pharmacist should keep in mind while dealing with his trade:
(i) Price structure
The prices charged should be fair keeping with the quality, quantity and labour or skill required.
(ii) Fair trade practice
Fair practice should be adopted by a pharmacist in the trade without any attempt to capture other pharmacist’s business.
If a customer brings a prescription (by mistake) which should be genuinely by some other pharmacy the pharmacist should refuse to accept the prescription.
Imitation of copying of the labels, trademarks and other signs or symbols of other pharmacy should not be done.
(iii) Purchase of drugs
Pharmacists should buy drugs from genuine and reputable sources.
(iv) Advertising and Displays
The sale of medicines or medical appliances or display of materials in undignified style on the premises, in the press or elsewhere are prohibited.
Pharmacist in relation to medical profession
Following are the code of ethics of a pharmacist in relation to medical profession:
(i) Limitation of professional activity
The professional activity of the medical practitioner as well as the pharmacists should be confined to their own field only.
Medical practitioners should not possess drugs stores and pharmacists should not diagnose diseases and prescribe remedies.
A pharmacist may, however, can deliver first aid to the victim in case of accident or emergency.
(ii) Cladenstine arrangement
A pharmacist should not enter into a secret arrangement or contract with a physician by offering him any commission or any advantages.
(iii) Liasion with public
A pharmacist should always maintain proper link between physicians and people. He should advise the physicians on pharmaceutical matters and should educate the people regarding health and hygiene.
The pharmacist should keep himself / herself up-to-date with pharmaceutical knowledge from various journals or publications.
Pharmacist in relation to his profession
Regarding to the profession the following code of ethics should be fulfilled.
(i)Professional vigilance
A pharmacist must abide by the pharmaceutical laws and he/she should see that other pharmacists are abiding it.
(ii)Law-abiding citizens
The pharmacists should have a fair knowledge of the laws of the country pertaining to food, drug, pharmacy, health, sanitation etc.
(iii)Relationship with Professional Organizations
A pharmacist should be actively involved in professional organization, should advance the cause of such organizations.
(iv)Decorum and Propriety
A pharmacist should not indulge in doing anything that goes against the decorum and propriety of Pharmacy Profession.
Pharmacist’s Oath
A young prospective pharmacist should feel no hesitation in assuming the following pharmacist’s oath:
- “I promise to do all I can to protect and improve the physical and moral well-being of society, holding the health and safety of my community above other considerations. I shall uphold the laws and standards governing my profession, avoiding all forms of misinterpretation, and I shall safeguard the distribution of medical and potent substances.
- Knowledge gained about patients, I shall hold in confidence and never divulge unless compelled to do so by law.
- I shall strive to perfect and enlarge my knowledge to contribute to the advancements of pharmacy and the public health.
- I furthermore promise to maintain my honour in all transactions and by my conduct never bring discredit to myself or to my profession nor to do anything to diminish the trust reposed in my professional brethren.
- May I prosper and live long in favour as I keep and hold to this, my Oath, but if violated these sacred promises, may the reverse be my lot.”
Scope and Potential of Pharmacy – Table Format
| Qualification | Area | Opportunities |
|---|---|---|
| General | Business | 1. Drug Store 2. Wholesale 3. Repacking 4. Bulk Drug Distribution 5. Cosmetic Manufacturing |
| D. Pharm | Service | 1. Hospital Pharmacy 2. Chemist in Drug Store / Wholesale Store 3. Medical Representative 4. Packaging, Store Maintenance in Pharmaceutical Industry 5. Secretary / PA to MD in Pharma Industry |
| Business | 1. Pharmaceutical Industry 2. Bulk Drug Manufacturing 3. Pharmacist Job Abroad 4. Cultivation of Medicinal Plants 5. Public Testing Laboratories 6. Consultancy | |
| B. Pharm | – | Same as D. Pharm with higher-level responsibilities and entry to R&D and QA/QC roles |
| M. Pharm | – | Eligibility for Teaching (Graduate Level), Advanced R&D, Regulatory Affairs, etc. |
| Ph.D. | Academic & Industry | 1. FDA Job 2. Teacher for Diploma Courses 3. Production 4. Marketing 5. Teacher for Graduate-Level Courses 6. Research and Development |
Conclusion
The History of Pharmacy in India showcases a profound shift—from plant-based traditional healing to globally recognized pharmaceutical excellence. With pioneers like Prof. Schroff, legislative reforms, and strong institutions, India has become a leader in drug manufacturing and research. The journey of the History of Pharmacy in India continues with innovation, education, and global integration at its core.
External Links
- Pharmacy Council of India (PCI) – pci.nic.in
- Indian Pharmacopoeia Commission (IPC) – ipc.gov.in
- Ministry of AYUSH – ayush.gov.in
- World Health Organization – Essential Medicines – who.int/medicines